Endocrine Unit, Department of Clinical Therapeutics and Evgenidion Hospital, Athens University School of Medicine, Athens Greece
Although the association of thyroid disorders with tuberculosis has been known for a long time, the diagnosis of thyroid tuberculosis is rare. Differential diagnosis can be very difficult without fine needle aspiration. The clinical course of the disease may resemble toxic goiter or acute thyroiditis or may follow a subacute or chronic pattern without specific symptomatology. We describe a 49-year old male patient with thyroid tuberculosis presenting as thyroid enlargement, fever, increased erythrocyte sedimentation rate, normal thyroid function tests, and a chest x-ray indicating the presence of a lesion with distinct calcification in the lower lobe of the right lung. Tuberculosis of the thyroid gland, although very rare, should be considered as a possible diagnosis when localized swelling, cold abscess or thyroid nodule with or without a cystic component are present.
Fine needle aspiration, Thyroid tuberculosis, Thyroiditis
INTRODUCTION
Tuberculosis of the thyroid gland is very rarely diagnosed.1-3 It was first reported in 1862 by Lebert1 in a patient with disseminated mycobacterial infection. The first case of primary thyroid infection, presenting as a rapidly enlarging goiter with cervical lymphadenopathy but no evidence of pulmonary tuberculosis, was reported in 1893 by Bruns.3 In 1926 five cases of thyroid tuberculosis were recognised by Coller and Huggins2 among 1200 thyroidectomies. In 1932 Rankin and Graham3 reported 21 cases out of 20,758 partial thyroidectomy specimens from the Mayo Clinic covering the period from 1920 to 1931, while in 1952 only two cases were identified by Levitt among 2114 consecutive thyroid specimens.4
Since then two studies involving fine needle aspiration cytology (FNAC) were conducted and lesions compatible with thyroid tuberculosis were found in 8 out of 1283 and in 18 out of 1565 cases, respectively.1,2 The exact number of cases reported is difficult to determine, but to our knowledge at least 186 cases (including our case) can be found cumulatively in the English language literature, four of which were children.5-8,12 Similarly, the true incidence of tuberculous thyroiditis is difficult to estimate possibly due to escape of the etiologic diagnosis.13
Establishing the diagnosis of thyroid tuberculosis is in most cases a challenge, since the lesion can often be mistaken for carcinoma, suppurative abscess or hemorrhage into a thyroidcyst. The clinical presentation is variable and usually consists of local symptoms related to enlargement of the gland, while thyroid function is rarely affected.14 Before the application of fine needle aspiration(FNA)as a method of investigating thyroid nodules, all the patients underwent surgical removal of the thyroid lesion (suspected of representing a tumor) and diagnosis was established by demonstration of tubercle bacilli in the biopsy specimens.
A case of thyroid tuberculosis in a 49-year old male patient is herein presented, possibly denoting reactivation of a latent pulmonary mycobacterial infection.
PATIENT DESCRIPTION
A 49-year old man presented with a slightly painful neck swelling. A fortnight previously he had sustained a high-grade fever (up to 40°C) which lasted for a week and subsided with paracetamol. He reported a subsequent intermittent low-grade fever and no further tenderness in the neck. He also reported a 2kg weight loss and increased palpitations and sweating. At presentation he had thyroid enlargement, mostly of the right lobe. A large hard nodule (>4cm) was palpable on the right lobe which was mildly tender. The heart rate was 88/min, the blood pressure was 135/80 mmHg and the tempera ture was 37.3oC.
Thyroid function tests which were performed at the time were normal: serum thyroid stimulating hormone (TSH) 1.09µUI/ml, thyroxine (T4) 79nmol/L, triiodothyronine (T3) 0.77nmol/L, FT4 16.12pmol/L FT3 4.3pmol/L and thyroglobulin (Tg) 190ng/ml. Anti-Tg and anti-thyroid peroxidase (TPO) antibodies were also normal. The blood count was as follows: hematocrit 41%, hemoglobin 12.8g%, platelets 268000/mm3, WBC 6800/mm3, with normal differential. Erythrocyte sedimentation rate (ESR) was 79mm/h and C reactive protein (CRP) was 120mg/dl (normal value <0.5mg/dl). A thyroid ultrasonography was performed which showed heterogeneity and the presence of a hypoechogenic nodule on the lower part of the right lobe, with a diameter of 55mm. The nodule was heterogeneous and had cystic degeneration(Figure1). AFNAwasperformedwhichshowed inflammatory cells and no signs of malignancy.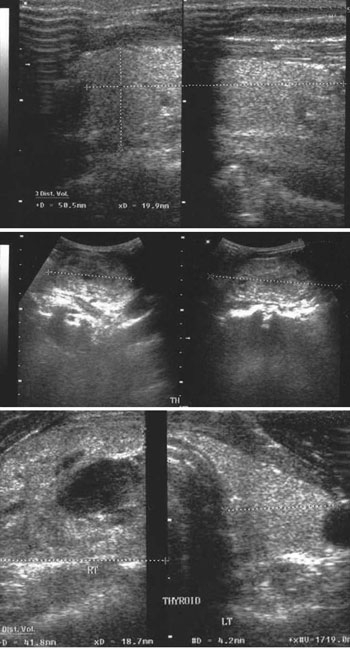
Figure 1. Thyroid ultrasound showing heterogeneity and the presence of a nodule on the lower right lobe, measuring 55mm. The nodule is heterogeneous and hypoechogenic and has cystic degeneration.
A chest x-ray (Figure 2) and a computed tomography (CT) of the chest showed a lesion with distinct calcification in the basal region of the right lower lobe. No other focal lesion was observed in the remaining pulmonary parenchyma. A heterogeneous nodule of the right thyroid lobe with irregular margins was again visualized in the CT, causing mild displacement of the trachea without infiltration. No lymph node enlargement was present.
Figure 2. Patient’s chest x-ray showing a lesion with distinct calcification in the lower lobe of the right lung. No other focal lesion is observed in the remaining pulmonary parenchyma.
Two weeks later the patient was almost afebrile, but the thyroid nodule showed some further enlargement. On the basis of this clinical course the patient underwent thyroidectomy. Pathologic examination showed an enlarged thyroid gland weighing 60 grams; multiple nodules were present with a diameter of 0.6-4.0cm. The largest hyperplastic nodule in the right lobe had a diameter of 4cm. Within this nodule as well as in a 0.6cm nodule of the left thyroid lobe a granuloma was present with epithelial cells and a central “caseous” necrosis. These morphological signs were compatible with multiple tuberculous foci of the thyroid gland. No signs of malignancy were present. It was not considered necessary for the patient to receive antituberculous treatment, as the lesion was totally excised and the chest x-ray findings did not show any signs of active disease.
DISCUSSION
Tuberculosis may affect the thyroid gland via either the haematogenous or the lymphogenous route or by direct invasion from the larynx or cervical lymph nodes.7 Focal caseous tuberculosis is the usual result of thyroid involvement, presenting as a localized swelling, cold abscess3 or thyroid nodule with or without acystic component.7,8,15 Alternatively, miliary spread to the thyroid may occur as a result of disseminated mycobacterial infection leading to the formation of multiple tubercles within the gland.
The clinical course of tuberculous thyroiditis is usually diverse. At presentation, the clinical picture resembles that of acute infectious thyroiditis. Patients present with pain and tenderness in the affected lobe or the entire gland and very occasionally with fever and chills.16,17 Apart from such a presentation, tuberculous thyroiditis may follow a subacute course resembling subacute granulomatous thyroiditis (De Quervain’s) or that of chronic non-suppurative thyroiditis. On rare occasions it can present as fever of unknown origin. Thyroid function tests usually remain within the normal limits or else euthyroid sick syndrome is demonstrated. Occasionally tuberculous thyroiditis is accompanied by thyrotoxicosis18-20 or hypothyroidism.21,22 Patients with subnormal immune response (HIV infection or use of immunomodulating drugs) usually present with atypical clinical (miliary forms) and histological (lymphocyte infiltration or atrophy) patterns of tuberculosis.
While tuberculous thyroiditis is a rare condition, it is also one that frequently may go un-or misdiagnosed. A chest x-ray and a tuberculin skin test (PPD) should be performed if mycobacterial infection is suspected. An accurate method to confirm the diagnosis is FNA of the thyroid gland. Definite diagnosis is established by characteristic histological findings such as epithelial cell granulomas with central caseous necrosis, peripheral lymphocytic infiltration and Langhans giant cells. In fact, caseous necrosis is a cytologic finding specific to tuberculosis. The simultaneous demonstration of acid fast bacilli (AFB) makes diagnosis almost certain. On the other hand, the smear may not reveal AFB positive staining,butthisfactdoesnotprecludethediagnosisifthe histological features and the clinical presentation are compatible.23 In such cases, results from the cultures (lasting 4-6 weeks) should be waited for.
The imaging techniques are not very helpful in establishing the diagnosis of tuberculous thyroiditis. Ultrasonography usually reveals a heterogeneous, hypoechoic mass similar to a neoplastic lesion. Contrast-enhanced CT may help localize the caseous necrotic lesion. This finding consists of a necrotic center with a peripheral rim enhancement due to acute inflammation causing thickening of adjacent tissues (“dermal sign”).24
The differential diagnosis of tuberculous thyroiditis depends on the presence or absence of local pain. If pain is the predominant clinical finding, the differential diagnosis lies between an infectious form of thyroiditis (bacterial, fungal, etc) and subacute granulomatous thyroiditis (De Quervain’s, thyroid sarcoidosis, etc). The culture of aspiration material and the distinct histological findings confirm the diagnosis of tuberculous thyroiditis. De Quervain’s thyroiditis may have similar histopathological features with thyroid sarcoidosis and thyroid tuberculosis but caseous necrosis is absent.
In the event that pain is absent, thyroidtuberculosis might be falsely diagnosed as thyroid malignancy; these conditions may even coexist.25 Rarely a tuberculous abscess of the supra-sternal notch region may cause dysphagia and mimic an anterior neck mass or thyroid tumor.
Treatment of thyroid tuberculosis consists of antituberculous drugs combined with surgical removal of the affected parts of the thyroid gland7 or surgical drainage.15 Lately it has been recognized that antituberculous drugs alone could be efficacious.22,26 A combination drug therapy consisting of isoniazid, rifampicine and vitamin B6 with or without the addition of ethambutol or a fluoroquinolone seems to be effective. This can lead to significant clinical improvement and avoidance of surgery in the event that preoperative diagnosis is established.12 Finally, if a thyroid tuberculous abscess is present, drainage combined with antituberculous drug therapy is considered as sufficient and further surgery is rarely required.27
In our patient,total thyroidectomy was performed, which took care of the nodular goiter as well. It was not considered necessary for the patient to receive anti-TBC treatment as the chest x-ray findings did not show any signs of active disease.
REFERENCES
1. Mondal A, Patra DK, 1995 Efficacy of fine needle as piration cytology in the diagnosis of tuberculosis of the thyroid gland: a study of 18 cases. J Laryngol Otol 109: 36-38.
2. Das DK, Pant CS, Chachra KL, Gupta AK, 1992 Fine needle aspiration cytology diagnosis of tuberculous thyroiditis. A report of eight cases. Acta Cytol 36: 517- 522.
3. Simkus A, 2004 Thyroid tuberculosis. Medicina (Kaunas) 40: 201-204.
4. Lebert H, 1862 Die Krankheiten der Schilddruse and Ihre Behandlung. Breslau 264.
5. Coller FA, Huggins CB, 1926 Tuberculosis of the thyroid gland. Ann Surg 84: 408.
6. Rankin FW, Graham AS, 1932 Tuberculosis of the thyroid gland. Ann Surg 96: 625.
7. Balasarkar D, Dhareswar J, Satoskar RR, Awsare N, Mahey R, Kumar V. Primary thyroid tuberculosis. Available from URL: http://bhj.org/journal/2000_4201_jan00/ case_trial.htm
8. Sadykov FG, Mukhtarov RS, 1987 Local form of tuberculosis of the thyroid gland in children. Vestn Khir Im I I Grek 139:114.
9. Surer I, Ozturk H, Cetinkursun S, 2000 Unusual presentation of tuberculosis reactivation in childhood: an anterior neck mass. J Pediatr Surg 35: 1263-1265.
10. Scott JX, Gnananayagam JE, Sundaravalli EK, Thomas G, Shanthly N, Kirubakaran C, 2004 Unusual cause for miliary lung mottling in a child. Indian J Chest Dis Allied Sci 46: 291-293.
11. Abdullah MA, Saleem MS, Salihi H, Hamid FA, Asaaf H, 1996 Tuberculous anterior neck mass simulating goitre. Ann Trop Paediatr 16: 369-371.
12. Pazaitou K, Chrisoulidou A, Ginikopoulou E, Angel J, Destouni C, Vainas I, 2002 Primary tuberculosis of the thyroid gland: report of three cases. Thyroid 12: 11371140.
13. Balacheff-Carrara O, Ozenne G, Ducastelle T, Jeuffroy P, Testart J, Wolf LM, 1984 [Thyroid tuberculosis: rare disease or rarely diagnosed?] Rev Med Interne 5: 229 230.
14. Tan KK, 1993 Tuberculosis of the thyroid gland-a review. Ann Acad Med Singapore 22: 580-582.
15. Talwar VK, Gupta H, Kumar A, 2003 Isolated tuberculous thyroiditis. JIACM 4: 238-239.
16. Larsen PR, Davies FT “Hypothyroidism and thyroiditis”. In: Williams Textbook of Endocrinology 10th edition. Saunders; p, 448.
17. Fung LM, Ma RC, Chow CC, Cockram CS, 2004 Infective thyroiditis in two cases of systemic lupus erythematosus. Hong Kong Med J 10: 344-346.
18. Nieuwland Y, Tan KY, Elte JW, 1992 Miliary tuberculosis presenting with thyrotoxicosis. Postgrad Med J 68: 677-679.
19. Kapoor VK, Subramani K, Das SK, Mukhopadhyay AK, Chattopadhyay TK, 1985 Tuberculosis of the thyroid gland associated with thyrotoxicosis. Postgrad Med J 61: 339-340.
20. Khan EM, Haque I, Pandey R, Mishra SK, Sharma AK, 1993 Tuberculosis of the thyroid gland: a clinicopathological profile of four cases and review of the literature. Aust N Z J Surg 63: 807-810.
21. Barnes P, Weatherstone R, 1979 Tuberculosis of the thyroid: two case reports. Br J Dis Chest 73: 187-191.
22. Milcu SM, Spandonide T, Saim A, 1981 Tuberculous thyroiditis cured by drug therapy. Endocrinologie 19: 261-263.
23. Khalil EA, Elsiddig KE, Elsafi ME, et al, 2000 Supra-sternal notch tuberculous abscess: a report of three cases. Trans R Soc Trop Med Hyg 94: 58-60.
24. Kang BC, Lee SW, Shim SS, Choi HY, Baek SY, Cheon YJ, 2000 US and CT findings of tuberculosis of the thyroid: three case reports. Clin Imaging 24: 283-286.
25. Suri VS, Sakhuja P, Malhotra V, Gondal R, Singh S, Sidhu N, 2002 Co-existent tuberculosis and papillary carcinoma thyroid. Trop Doct 32: 118.
26. Orlandi F, Fiorini S, Gonzatto I, et al, 1999 Tubercular involvement of the thyroid gland: a report of two cases. Horm Res 52: 291-294.
27. el Malki HO, el Absi M, Mohsine R, et al, 2002 [Tuberculosis of the thyroid. Diagnosis and treatment]. Ann Chir 127: 385-387.
Address for correspondence:
Maria Alevizaki MD PhD, Associate Professor in
Endocrinology, Athens University School of Medicine, 51,
Ioannou Theologou Str, 157 73 Athens, Greece, fax+30-210
7704143, e-mail, mani@otenet.gr
Received 22-05-06, Revised 14-09-06, Accepted 10-11-06