1İzmir Bozyaka Training and Research Hospital, Department of Internal Medicine, 2Ege University, Division of Endocrinology and Metabolism, 3İzmir Bozyaka Training and Research Hospital, Division of Endocrinology and Metabolism; İzmir, Turkey
Hypokalemia, Periodic paralysis, Thyrotoxicosis, U wave
Dear Editor,
Hypokalemic periodic paralysis (HPP) is a rare neuromuscular disorder caused by dysfunction of the ion channels in red muscle cells and which is characterized by painless episodes of muscle weakness generally after strenuous exertion or a high-carbohydrate meal.1 Most HPP cases are hereditary since the disease is autosomal dominant. However, some patients who develop HPP secondary to thyrotoxicosis are also described. Thyrotoxic hypokalemic periodic paralysis (THPP), unlike other thyroid diseases, is predominantly seen in men.2 Here we report the case of a patient with no known chronic illness who presented with paralysis and who was subsequently diagnosed as having thyrotoxicosis with hypokalemic periodic paralysis being caused by his thyroid disease.
A 41-year-old Caucasian man, without any chronic disease, presented to our emergency department with generalized muscle weakness that was especially pronounced in both his upper and lower extremities. He recalled many similar but milder episodes in the previous two months. The physical examination made by a neurologist identified no pathology but only quadriparesis (bilateral upper extremities 3/5, bilateral lower extremities 4/5). His initial potassium level was 1.5 mEq/L on admission and his electrocardiogram showed an obvious U wave (Figure 1). An initial diagnosis of hypokalemic periodic paralysis was made and he was immediately given intravenous potassium chloride in the emergency department. He was then interned and, after he had been provided a detailed anamnesis, it was learned that he had no family history like his own and that he had had a high-carbohydrate meal a few hours before the quadriparesis occurred. On admission, blood pressure was 140/80 mmHg and heart-rate 90 beats/minute. Physical examination revealed a slightly enlarged thyroid gland without nodules, while exophthalmoswas also present. The clinical findings of other systems were normal. Thyroid stimulating hormone (TSH) level was <0.03 μU/mL (0.25–5.0), free thyroxine level (fT4) 4.21 ng/dL (0.77–1.71), and free tri-iodothyronine (fT3) 19.55 ng/dL (0.23-0.39), anti-thyroid peroxidase antibodies (anti-TPO) 2261 IU/mL (<9.0 IU/mL). Thyroid ultrasound showed that the left lobe measured 27×28×29mm, while the right lobe measured 35×31×30mm. The gland appeared enlarged and heterogeneous in texture. Internal septations were observed. Thyroid scintigraphy led us to diagnose Graves’ disease.
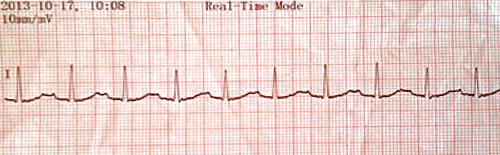
Figure 1.
Electrocardiogram of the patient.
On the basis of these findings, the patient was diagnosed as having THPP associated with Graves’ thyrotoxicosis, and treatment with methimazole was initiated. Serial measurements of his serum potassium level, which was too low on admission and then became normal after administration of intravenous potassium chloride, remained within normal limits without any oral potassium supplementsin the hospital. Treatment with propranolol was also initiated at 4×40mg per day and the patient was discharged with the diagnosis of THPP secondary to Graves’ disease.
THPP is a sporadic form of HPP and occurs in association with hyperthyroidism. In most cases of THPP, the main underlying cause is Graves’ disease. More than 95% of THPP cases are seen in men, despite the greater tendency of women to have thyroid diseases. The pathogenesis of THPP, which is a rare complication of thyrotoxicosis causing hypokalemia only during episodes, is the activation of the Na+/K+-ATPase pump because of hyperinsulinemia and the increase of thyroid hormones, catecholamines and beta-adrenergic stimulation. Besides these latter factors, resting after exercise can also increase Na+/K+-ATPase activity in skeletal muscle, promoting an influx of potassium.3,4 Therefore, B receptor blockage, anti-thyroid drugs and instructing patients to avoid such precipitating factors as high-carbohydrate meals are recommended for treatment and prophylaxis of THPP instead of administering potassium only.5 Unless there are cardiopulmonary complications, KCl infusion should be given, however, at a slow rate because it may result in rebound hyperkalemia as potassium shifts back into the intravascular compartment.6
The aim of this letter is to share this case of THPP in a patient, who, like most patients described in the literature, was not aware of his thyroid disease. By presenting this case, we wish to emphasize the importance of carrying out a good anamnesis and physical examination, which will lead to a right diagnosis and successful treatment.
FUNDING
None of the authors has any conflict of interest.
REFERENCES
1. Miller JD, Quillian W, Cleveland WW, 1997 Non familial hypokalemic periodic paralysis and thyrotoxicosus in a 16-year old male. Pediatrics 100: 412-414.
2. Vijayakumar A, Ashwath G, Thimmappa D, 2014 Thyrotoxic periodic paralysis: clinical challenges. J Thyroid Res 2014: 649502.
3. Hsieh MJ, Lyu RK, Chang WN, et al, 2008 Hypokalemic thyrotoxic periodic paralysis: clinical characteristics and predictors of recurrent paralytic attacks. Eur J Neurol 15: 559-564.
4. Erem C, 2005 Thyrotoxic hypokalemic periodic paralysis in a Turkish male with Graves’ disease: a rare case report and review of the literature. Endocrine 27: 63-65.
5. Kung AW, 2006 Clinical review: Thyrotoxic periodic paralysis: a diagnostic challenge. J Clin Endocrinol Metab 91: 2490-2495.
6. Lu KC, Hsu YJ, Chiu JS, et al, 2004 Effects of potssium supplementation on the recovery of thyrotoxic periodic paralysis. Am J Emerg Med 22: 544-547.
Address for correspondence:
Banu Sarer Yurekli, Ege University, Division of Endocrinology and Metabolism, İzmir, Turkey, Ege University Hospital, Department of Endocrinology, Bornova, 35100, Izmir, Turkey; Mobile: +905055250373, Fax: +902323472388, E-mail: bsareryurekli@yahoo.com
Received:10-05-2016, Accepted:12-05-2016