1Postgraduate Course Stress Management and Health Promotion, Athens University Medical School; 21st Department of Propedeutic Medicine, Athens University Medical School, "Laiko" General Hospital; 32nd Department of Pediatrics, Athens University Medical School, "P. & A. Kyriakou" Children’s Hospital; 41st Department of Pediatrics, Athens University Medical School, "Aghia Sophia" Children’s Hospital; Athens, Greece
OBJECTIVE: Although there is scientific evidence that stress adversely affects metabolic control, only a few studies have examined the role of stress management in improving glycemic control in patients with type 2 diabetes mellitus (DM). In this study, we investigated the effect of a relaxation technique on levels of stress and glycemic control.
DESIGN: A total of 53 patients with type 2 DM were randomly assigned to undergo either an 8-week stress management program, consisting of 10 min of diaphragmatic breathing and 15 min of progressive muscle relaxation twice per day (n=25, intervention group), or not (n=28, control group). Perceived stress, health locus of control and HbA1c were primary outcomes and were measured before and after intervention.
RESULTS: In the intervention group, perceived stress score (PSS) and HbA1c had decreased significantly (P<0.05) by the end of the program. Specifically concerning the PSS, the higher the initial levels of perceived stress the greater the benefit of the intervention. No other significant changes were found.
CONCLUSIONS: Our results show a beneficial role of stress management for patients with type 2 DM, as regards both stress levels and glycemic control. It is recommended to consider this type of treatment as an adjunct to conventional therapy. We deem that our study could encourage future studies in this area with larger samples, longer duration and more objective measurements.
Diabetes type 2, HbA1c, Intervention, Perceived stress, RCT, Stress management
INTRODUCTION
Diabetes mellitus is a heterogeneous group of metabolic diseases characterized by chronic hyperglycemia and metabolic disorders, with type 2 diabetes being the most common form.1 Obesity and physical inactivity were identified early on as significant causal factors1-3 but only recently has stress been implicated in its pathology as well. Chronic activation of the hypothalamic pituitary axis (HPA) can lead to severe metabolic consequences, common in visceral obesity and metabolic syndrome.4-7 At the same time, diabetes itself can add to the initial stress burden not only due to the actual level of glycemia but also because of the pressure incurred by lifestyle modification and the insulin injection.
Therefore, many studies have tried to assess whether stress management can have a beneficial role in the management of patients with type 2 diabetes. Regarding stress reduction, the few available studies show that cognitive behavioral therapy (CBT),8,9 meditation and biofeedback appear to be effective.10,11 In terms of improving glycemic control, results have been mixed: some have found a positive effect,9-11 while others have not.8-12
One of the most popular stress management techniques is progressive muscle relaxation (PMR),13 which incorporates both a physical and a mental component. The knowledge of relaxation breathing (RB) is usually required for proper application. According to research data, the combination of this technique (RB-PMR) with others (biofeedback, guided imagery, CBT) has shown a beneficial effect in lowering stress levels,8,9,14 though a positive metabolic action has not yet been demonstrated.10,12
In summary, it is clear that the literature is as yet inadequate and the results of the few available studies mixed, especially regarding the effect of this technique on glycemic control. While there is still no systematic review of randomized clinical trials that have used PMR-RB to improve glycemic control in patients with type 2 diabetes, at the same time its combination with other techniques makes it difficult to draw conclusions about its effectiveness.
The primary aim of this study is to add to the literature by investigating the effects of RB-PMR on HbA1c, perceived stress (PSS) and health locus of control (HLC subscales). Secondary endpoints include the identification of changes in stress related symptoms, saliva cortisol, a putative dose-response effect, stress predictors and factors affecting compliance.
SUBJECTS AND METHODOLOGY
This was a parallel group, randomized, controlled trial with an almost 1:1 allocation ratio of treatment or non-treatment groups and 8 weeks of follow-up. After trial commencement there were a few deviations from original protocol (e.g. exclusion criteria, patient contact frequency).
The study was conducted in cooperation with the outpatient Diabetes Clinic of Laiko General Hospital in Athens, Greece, between November 2011 and July 2012. Recruitment was performed on the same days twice per week, from November 2011 till May 2012. All participants were fully informed about the purposes of the study and provided written consent. The study had the approval of the Scientific Committee of our hospital. Meetings with patients were one-on-one and were held in a specific area ceded to the researcher after an agreement between the Diabetes and Dietetics Departments. Eligible participants were all patients diagnosed with type 2 diabetes according to the criteria of the American Diabetes Association, who lived in Athens, were aged 30-75 years and were under the conventional treatment (diet, exercise, antidiabetic drugs and insulin). Exclusion criteria included diagnosis of type 1 diabetes mellitus, current neuroleptic or psycho-stimulant medication or psychiatric treatment, the use of corticosteroids within the last month, practice of other relaxation technique(s), significant acute or chronic concomitant disease, serious diabetes complications (e.g. severe visual impairment), end-stage renal disease and amputation, poorly controlled diabetes [glycated hemoglobin A1c (HbA1c)] >8.5%, (>68mmol/mol)], pregnancy, breastfeeding and incompetence at reading or writing in Greek. After enrollment, participants who changed their type or dose of diabetes medication or insulin or experienced an objectively severe stressful event (one or more of the first five events of the Social Readjustment Rating Scale) were also excluded from the analysis to avoid bias.
After an initial screening of each patient’s file information, they were contacted and informed about the study. For those patients who declined to participate, the reasons were recorded. Patients who were interested to learn more were invited to the hospital for the first meeting so as to confirm eligibility and describe study requirements. Eligible participants were randomly assigned to either the intervention or the control group. A simple randomization procedure (random numbers generated by an online generator, www.random.org) was used. Randomization, baseline and final measurements were not blinded. On the other hand, data analysis was blinded. All information (e.g. effects of stress on health, instructions for saliva cortisol sample and questionnaires) were provided in an identical verbal and written manner. When the first questionnaires had been completed, HbA1c was measured and a saliva cortisol sample was taken at the second meeting. In the treatment group, RB-PMR was provided by an audio CD comprising 10 min of DB (deep breathing) and 15 min of PMR. Practice of some exercises and explanation of the RB-PMR philosophy and health benefits followed. All patient questions were answered. Patients were encouraged to focus on the difference between stress and relaxation through different muscle groups so as to increase their perception of relaxation response.13 In addition, they were asked to practice the technique twice a day for 8 weeks and keep a diary. When the technique was not performed, reasons were recorded. To measure and enhance compliance and eliminate dropouts, participants in the intervention group were contacted on a weekly basis. During the telephone communication, patients were asked to report on any problems when practicing RB-PMR and the principal sources of stress during the last week as well as to make general comments, all of which were recorded. No counseling was provided during the telephone communication. At the end of the intervention 8 weeks later, the final questionnaires and cortisol samples were returned and HbA1c was measured. Finally, the control group continued with the usual care of the hospital department (physician and dietitian meeting) and at the end of the intervention participants were rewarded with a relaxation CD.
Baseline and outcome measures included the following:
Sociodemographic characteristics (sex, age, marital status, educational level (years of education), place of residence (now and in the past), job schedule and self-reported financial status.
Medical history: Diabetes duration, type and dose of medication or insulin, occurrence of hyperlipidemia, hypertension or thyroid disease, other serious health problems, smoking status.
Lifestyle disease related factors: Body mass index (BMI), waist-to-hip ratio (WHR), physical activity status (type, frequency, intensity), adherence to the Mediterranean diet using the MedDietScore.15
Stress levels: The Perceived Stress Scale is a measure of the degree to which an individual’s situations in life are appraised as stressful.16 Questions are designed in such a way that a person may evaluate how unpredictable, uncontrollable and overloaded he perceives his life to be. At the same time, there are questions that evaluate the levels of experienced stress directly. Participants were also asked about stress symptoms, both physical and psychological, through a specific list. Finally, the Social Readjustment Rating Scale (SRRS),17 consisting of 43 life events which are considered stressful, was completed. Each event has a numerical value. As mentioned above, the scale was used as a criterion for exclusion from the statistical analysis for patients who had experienced one of the first five listed events over the past 2 months.
Health Locus of Control (HLC subscales)18 validated in Greek.19 Individuals express their degree of agreement to 18 proposals on a 6-grade Likert scale. The scale consists of three subscales, independent of each other. The internal subscale reflects the degree to which a person believes that he/she is responsible for his/her health. The external subscale and the luck-related subscale represents the extent to which other people (e.g. doctors, family) or luck, respectively, are perceived as the main determinants of health. The higher the score on each subscale, the stronger the belief in that determinant.
Laboratory data: HbA1c, an indicator of metabolic control for the past 3 months, was measured with high pressure liquid chromatography (HPLC). Saliva cortisol samples were also taken to determine stress levels. The secretion of cortisol is pulsed (about 15 beats a day) and its concentration in the blood fluctuates daily. The highest level occurs 30-45 min after awakening and is noted on the curve as CAR (Cortisol Awakening Response). Subsequently, a gradual decline can be observed until the evening, this reduction rate being described as the daily slope (diurnal slope). The average daily concentration of cortisol throughout the day is described by the area under the curve (Area Under the Curve-AUC). In this study we used the shortest protocol, which requires three measurements per day and has the largest application and reliability. The measurements were made immediately after awakening, and 45 minutes and 12 hours later, respectively (e.g. 08:00, 08:45 and 20:00).
For sample size calculation, we assumed a large attrition rate of 30% by week 8 during the intervention phase, primarily due to increased daily requirements. Therefore, we had anticipated needing at baseline 74 subjects (52 after dropouts) with type 2 diabetes to detect large effect sizes (effect size of 0.8 SD) with at least 80% power (statistical significance level a=0.05, allocation ratio almost 1:1). Following enrollment, the dropout exclusion rate at the stage of analysis was 28%, yielding a final sample of 53 patients.
For the presentation of the research data, the means ± standard deviation was used for continuous variables as well as the absolute and proportion frequencies for categorical variables. For group comparisons, Student’s t-test and the Mann-Whitney U-test were used, according to normality (assessed by Q-Q plots, histograms and the Kolmogorov-Smirnov or Shapiro-Wilk test), for continuous variables and the Chi-squared test for qualitative variables. Next, a modified per-protocol analysis was chosen because it contains less error compared to intention-to-treat analysis. Specifically, dropout reasons were about the same between the two groups and patients that were excluded from the analysis by the investigator reported severe stressors, which would have introduced bias.
Finally, in terms of statistical analysis, changes in HbA1c, PSS, HLC1, HLC2 and HLC3 scores were used as primary outcomes. To detect differences between groups, one-way analysis of covariance (ANCOVA) was used. All assumptions were checked. For PSS, HLC1, HLC2 and HLC3, the baseline values were used as covariates. For HbA1c, age, gender and baseline HbA1c were considered the most important covariates. PSS was not entered into the model due to moderate correlations with age (Spearman’s rho=-0.294, p=0.036) and sex (Spearman’s rho=0.312, p=0.026), which induces undesirable colinearity. Effect sizes were calculated for each variable using Cohen’s d. Generally, the effect sizes of 0.8, 0.5 and 0.2 are considered as large, medium and small, respectively. Secondary endpoints (changes in symptoms perception, dose-response effect, factors affecting compliance with the technique, saliva cortisol levels) were addressed with simple Spearman’s ρ correlation tests and the parametric Student’s t-test or non-parametric Mann-Whitney test, for numerical-by-numerical and numerical-by-nominal comparisons, respectively. The level of statistical significance was 5%. Statistical analysis was performed using SPSS for Windows (version 18.0.3) statistical software (SPSS Inc., Chicago, IL).
RESULTS
The study was conducted in 53 patients with type 2 diabetes referred to the outpatients’ Diabetes Clinic. The flowchart of the participants is displayed in Figure 1.
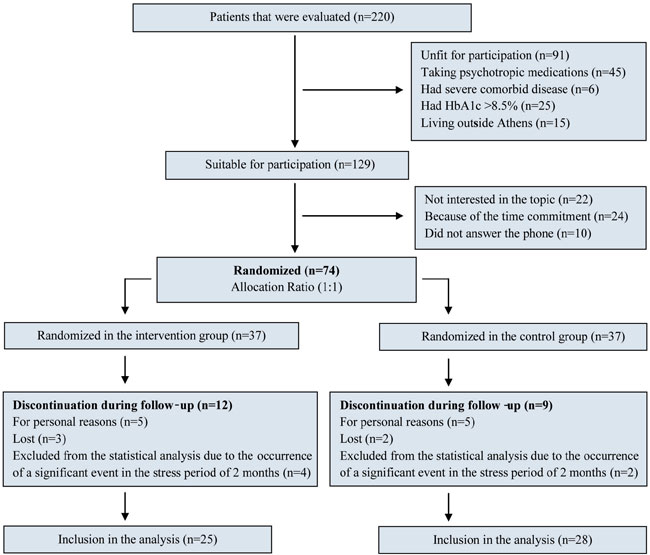
Figure 1. Flowchart of participants.
Table 1 shows the distribution of the sociodemographic, clinical and lifestyle characteristics of the participants. For categorical variables, absolute and relative frequencies (n, %) are used. For quantitative values, means or medians and standard deviations, depending on normal distribution assumption, are computed, respectively. Most of the participants were over 60, without a partner, overweight or obese, physically active, of moderate socioeconomic status, and none were current smokers. The majority took tablets rather than insulin. The mean baseline of PSS, HLC, cortisol levels and HBA1c are also presented. There were no significant baseline differences between the two study groups (p >0.05).
A significant decrease in PSS was observed in the intervention group with moderate effect size (Cohen’s d=0.71, p=0.011), after controlling for baseline PSS and interaction with the group (Table 2). After a visual graph assessment (Figure 2), it was apparent that the higher the initial levels of perceived stress, the greater the benefit of the technique for PSS scores >16. For PSS <16, there were not sufficient subjects to detect any potential relationship and this may be the reason for the interaction. As for HbA1c, moderate reduction with medium effect size (Cohen’s d=0.73, p=0.015) was observed after adjustment for age, gender, baseline HbA1c levels and age by group interaction. The interaction indicates that the mean HbA1c differences depended on patients’ age. As depicted in Table 2, the mean HbA1c change was calculated for patients of the same sex, aged 61.8 years and baseline HbA1c 6.7%. A further analysis was conducted, adding socioeconomic status as a covariate, and HbA1c reduction remained statistically significant (p=0.029) (data not shown). For HLC subscales, small non-significant differences were observed after controlling for baseline values and interactions between baseline levels and group.
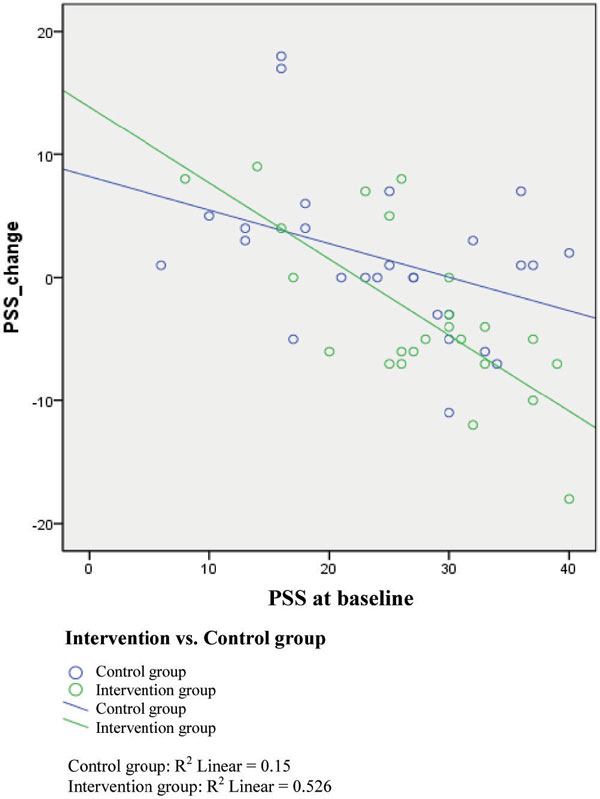
Figure 2. Correlation between changes in Perceived Stress Score between the two study groups. Patients with higher baseline stress levels practicing RB-PMR for 8 weeks showed a larger reduction in PSS.
Regarding secondary endpoints, a decrease in the average stress symptoms score was observed as well as in physical and psychological symptoms subscores. However, only the physical symptoms score mean change was significant (ΔPhys score=-3.25±6.11, p=0.023).
Next, cortisol profiles in the whole sample and in each group separately before and after the intervention were studied. At the beginning of treatment, the cortisol profile was not consistent with the normal daily variation (circadian pattern) in the whole sample and the intervention group. Post intervention, cortisol followed the familiar pattern of variation, with higher values seen in the morning and 30-45 minutes after the alarm in both groups. However, no statistically significant difference was recorded.
Spearman’s correlations of times of practice and primary outcomes were not significant (Spearman’s rho = 0.123 for ΔPSS, 0.085 for ΔHbA1c, 0.194 for ΔHLC1, 0.245 for ΔHLC2, 0.166 for ΔHLC3). Thus, no dose-response relationship was observed. As far as compliance with treatment is concerned, only individuals with increased BMI (Spearman’s rho=0.425, p=0.035) and shorter disease duration (Spearman’s rho=-0.463, p=0.034) were linearly associated with better compliance with relaxation treatment instructions.
Finally, it was examined whether certain variables (age, sex, level of education, use of insulin, diabetes history, socioeconomic level, number of children, body mass index, HbA1c, duration of diabetes mellitus, occupation, smoking habits) were associated with greater levels of stress. We found that men (Spearman’s rho=-0.312, p=0.026) and patients of higher socioeconomic status Spearman’s rho= -0.314, p=0.025) experienced less stress in relation to women and people of lower socioeconomic level, respectively.
DISCUSSION
This randomized clinical trial was conducted to evaluate the effect of stress management through an 8-week relaxation program. Our results can be summarized as the following: RB-PMR significantly reduced perceived stress and glycosylated hemoglobin with medium effect sizes recorded (Cohen’s d=0.71 and 0.67, respectively). In addition, higher baseline perceived stress was associated with greater PSS decrease. The three HLC subscales did not change significantly. Regarding stress symptoms, the physical, but not psychological, symptoms score decreased in the intervention group with moderate effect size (Cohen’s d=0.66). In addition, patients with diabetes in the intervention group practiced the relaxation technique 0.8 times per day. Patients with a higher BMI and the most recent diabetes diagnosis showed better compliance with the program. However, no dose-response relationship between times of practice and primary outcomes was noted. Furthermore, female gender and low socioeconomic level were linearly associated with higher perceived stress at the beginning of the intervention. Finally, the baseline cortisol profile was blunted in the intervention group; after intervention, the cortisol profile was normal in both groups. Mean cortisol changes were not statistically significant.
Regarding the effect of RB-PMR on stress levels in patients with type 2 diabetes, there are no recent research data. However, previous studies suggest that this technique, when combined with biofeedback and CBT, has beneficial effects on stress and anxiety levels.8-14 On the other hand, when provided along with guided imagery it does not seem to offer similar benefits.12 Perceived stress reduction is likely to be mediated by the short-term effects of RB-PMR, such as a reduced perception of pain, a pleasant mental status, stimulation of the parasympathetic system or a temperature increase.20 Long-term application has been associated with a decrease in cortisol saliva, generalized anxiety,21 blood pressure,21,22 heart rate40 and headaches.23
As far as the benefits of the technique in glycemic control are concerned, few studies have used this technique in individual sessions. Therefore, a “side by side” comparison with our own study is difficult. In agreement with our study, Surwit et al found that PMR in combination with CBT and diabetes education during five group sessions can reduce HbA1c by 0.5% (4mmol/mol).9 However, a previous study that used PMR and CBT during six group sessions did not find a statistically significant reduction in HbA1c.8 In another intervention in African women with type 2 MD, PMR was found to offer benefits similar to those of physical activity.24 Finally, some studies suggest that any benefits regarding glycemic control may not be detectable until after one year of intervention,9 or they may be restricted to specific groups of patients (i.e. those with elevated baseline anxiety, neuroticism, etc).12,25 In our study we did not test this particular case.
The effect of stress on metabolic activity has been thoroughly examined. Chronic activation of the HPA axis induces the release of count regulatory hormones (glucagon, epinephrine, cortisol), which affect the metabolic actions of insulin and lead to hyperglycemia.26,27 Moreover, cortisol, accompanied by an energy surplus, promotes mainly visceral obesity, which contributes to insulin resistance.27 Another mechanism implicates inflammation. Stress triggers an acute phase inflammatory response, a key component of the immune response, which is mediated by macrophages, the liver, adipose tissue, etc. and leads to cytokines overproduction (IL-1, IL-6, TNF-a).43 Finally, stress induces ischemia of the gastrointestinal tract, leading to increased intestinal permeability and endotoxemia, which aggravates existing inflammation.28,29
Regarding secondary outcomes, relief of physical symptoms can selectively be attributed to the nature of the technique, which is more muscle-oriented and includes no cognitive or behavioral elements.30 Furthermore, in agreement with other studies, female gender31,32 and low socioeconomic status33 were associated with higher PSS levels at the beginning of the intervention. Finally, the initially blunt cortisol profile in the intervention group is consistent with the findings of Bruehl et al.34 However, this condition did not last till the end of the intervention and changes in mean cortisol were not statistically significant.
It is acknowledged that this study has a number of limitations. First, our primary outcomes, PSS and HLC, were based on self-reports as opposed to clinical and/or laboratory assessments. Especially regarding PSS, there are a number of potential confounders (e.g. personality, psychopathology, beliefs, values and the current mood of the respondents) that can seriously modify the results.35 Furthermore, most secondary outcomes, like symptoms of stress, were based on non-validated questionnaires, which can introduce information bias as they may not measure what they are created for and disregard important elements of the population for which they are designed. In addition, the intervention group generally showed greater consistency to questionnaire instructions and were more prone to improve final results (e.g. misjudge stress symptoms, perceived stress). The lack of blindness and the inability to confirm compliance aside from the diary entries should not be ignored. Another important point is the fact that the study duration was based on the technique protocol (8 weeks). However, HbA1c is commonly tracked after a 12-week interval, so it is possible that the actual HbA1c change is not entirely depicted at week 8. Finally, there are no clinically meaningful cut-offs for perceived stress and secondary outcomes, thus the extrapolation of our results to clinical practice warrants caution. For this reason, sample size calculation was based solely on detecting high effect sizes.
The generalization of our results is limited to outpatients with type 2 diabetes without acute or severe coexisting disease, who live in an urban area and follow typical diabetes treatment. There are many reasons why this group of patients was chosen. Firstly, the technique requires the use of muscle groups; therefore, patients with limited motor activity (i.e. patients with peripheral neuropathy or vascular disease) were excluded. Secondly, only patients following a stable treatment plan were included (mean disease duration 8 years). By that time, current treatment (diet, medication) will have conferred its benefits, thus, the addition of a supplementary treatment is rational. On the other hand, patients with newly diagnosed diabetes were excluded from the study due to frequent medication or insulin adjustments.
Overall, this study provides additional evidence of the benefits of stress management for patients with type 2 diabetes on both physical and psychological levels. Further research with larger samples, longer duration and more objective outcomes are necessary to assess the utility of relaxation techniques. We deem that the implementation of simple techniques, such as RB-PMR, characterized by low cost, small time requirements and feasibility, should be considered a cost-effective, non-pharmaceutical adjunct treatment for patients with type 2 diabetes in everyday clinical practice.
FUNDING
There was no funding of this study.
CONFLICT OF INTEREST
None declared.
REFERENCES
1. The InterAct Consortium, 2012 Physical activity reduces the risk of incident type 2 diabetes in general and in abdominally lean and obese men and women: the EPIC-InterAct Study. Diabetologia 55: 1944-1952.
2. Kohrt WM, Kirwan JP, Staten MA, Bourey RE, King DS, Holloszy JO, 1993 Insulin resistance in aging is related to abdominal obesity. Diabetes 42: 273-281.
3. Ohlson LO, Larsson B, Svardsudd K, et al, 1985 The influence of body fat distribution on the incidence of diabetes mellitus. 13.5 years of follow-up of the participants in the study of men born in 1913. Diabetes 34: 1055-1058.
4. Wellen KE, Hotamisligil GS, 2005 Inflammation, stress, and diabetes. J Clin Invest 115: 1111-1119.
5. Friedman TC, Mastorakos G, Newman TD, et al, 1996 Carbohydrate and lipid metabolism in endogenous hypercortisolism: shared features with metabolic syndrome X and NIDDM. Endocr J 43: 645-655.
6. Kyrou I, Chrousos GP, Tsigos C, 2006 Stress, visceral obesity, and metabolic complications. Ann N Y Acad Sci 1083: 77-110.
7. Kyrou I, Tsigos C, 2007 Stress mechanisms and metabolic complications. Horm Metab Res 39: 430-438.
8. Henry J, Jane L, Wilson PH, Bruce DG, Chisholm DJ, Rawling DJ, 1997 Cognitive-behavioural stress management for patients with non- insulin dependent diabetes mellitus. Psychology, Health & Medicine 2: 109-118.
9. Surwit RS, van Tilbur MA, Zucker N, et al, 2002 Stress management improves long-term glycemic control in type 2 diabetes. Diabetes Care 25: 30-34.
10. Rosenzweig S, Reibel DK, Greeson JM, et al, 2007 Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Altern Ther Health Med 13: 36-38.
11. McGinnis RA, McGrady A, Cox SA, Grower-Dowling KA, 2005 Biofeedback-assisted relaxation in type 2 diabetes. Diabetes Care 28: 2145-2149.
12. Aikens JE, Kiolbasa TA, Sobel R, 1997 Psychological predictors of glycemic change with relaxation training in non-insulin-dependent diabetes mellitus. Psychother Psychosom 66: 302-306.
13. Jacobson E, 1938 Progressive Relaxation. Chicago, University of Chicago Press.
14. Jablon SL, Naliboff BD, Gilmore SL, Rosenthal MJ, 1997 Effects of relaxation training on glucose tolerance and diabetic control in type II diabetes. Appl Psychophysiol Biofeedback 22: 155-169.
15. Panagiotakos DB, Pitsavos C, Stefanadis C, 2006 Dietary patterns: a Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr Metab Cardiovasc Dis 16: 559-568.
16. Cohen S, Kamarck T, Mermelstein R, 1983 A global measure of perceived stress. J Health Soc Behav 24: 385-396.
17. Holmes TH, Rahe RH, 1967 The Social Readjustment Rating Scale. J Psychosom Res 11: 213-218.
18. Wallston KA, Wallston BS, DeVellis R, 1978 Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health Educ Monogr 6: 160-170.
19. Karademas EC, 2009 Effects of exposure to the suffering of unknown persons on health-related cognitions, and the role of mood. Health (London) 13: 491-504.
20. Titlebaum HM, 1988 Relaxation. Holist Nurs Pract 2: 17-25.
21. Pawlow LA, Jones GE, 2005 The impact of abbreviated progressive muscle relaxation on salivary cortisol and salivary immunoglobulin A (sIgA). Appl Psychophysiol Biofeedback 30: 375-387.
22. Sheu S, Irvin BL, Lin HS, Mar CL, 2003 Effects of progressive muscle relaxation on blood pressure and psychosocial status for clients with essential hypertension in Taiwan. Holist Nurs Pract 17: 41-47.
23. Anderson RE, Seniscal C, 2006 A comparison of selected osteopathic treatment and relaxation for tension-type headaches. Headache 46: 1273-1280.
24. van Rooijen AJ, Rheeder P, Eales CJ, Becker PJ, 2004 Effect of exercise versus relaxation on haemoglobin A1C in Black females with type 2 diabetes mellitus. QJM 97: 343-351.
25. Lane GD, McCaskill CC, Ross SL, Feinglos MN, Surwit RS, 1993 Relaxation training for NIDDM. Predicting who may benefit. Diabetes Care 16: 1087-1094.
26. Chrousos GP, 1998 Stressors, stress, and neuroendocrine integration of the adaptive response. The 1997 Hans Selye Memorial Lecture. Ann N Y Acad Sci 851: 311-335.
27. Morton NM, 2010 Obesity and corticosteroids: 11beta-hydroxysteroid type 1 as a cause and therapeutic target in metabolic disease. Mol Cell Endocrinol 316: 154-164.
28. Yang RB, Mark M, Gray A, et al, 1998 Toll-like receptor-2 mediates lipopolysaccharide-induced cellular signalling. Nature 395: 284-288.
29. Deitch EA, 1992 Multiple organ failure. Pathophysiology and potential future therapy. Ann Surg 216: 117-134.
30. Lehrer PM, Carr R, Sargunaraj D, Woolfolk RL, 1994 Stress management techniques: are they all equivalent, or do they have specific effects? Biofeedback Self Regul 19: 353-401.
31. Barbosa-Leiker C, Kostick M, Lei M, et al, 2012 Measurement Invariance of the Perceived Stress Scale and Latent Mean Differences across Gender and Time. Stress Health 29: 253-260.
32. Herrero SG, Saldana MA, Rodriguez JG, Ritzel DO, 2012 Influence of task demands on occupational stress: gender differences. J Safety Res 43: 365-374.
33. Rebbeck TR, Weber AL, Spangler E, Zeigler-Johnson CM, 2013 What stresses men? predictors of perceived stress in a population-based multi-ethnic cross sectional cohort. BMC Public Health 13: 113.
34. Bruehl H, Wolf OT, Convit A, 2009 A blunted cortisol awakening response and hippocampal atrophy in type 2 diabetes mellitus. Psychoneuroendocrinology 34: 815-821.
35. Herbert TB, Cohen S, 1996 Measurement issues in research on psychosocial stress. In: HB Kaplan (ed) Psychosocial stress: Perspectives on structure, theory, life-course, and methods, Academic Press, London; pp, 295-332.
Address for correspondence:
Efi Koloverou, ΜSc, PhD (candidate), 107 Sapfous Str., 176 76 Kallithea, Athens, Greece, Tel.: +302109532182, E-mail: efi.koloverou@gmail.com
Received 18-10-2013, Accepted 18-02-2014